Big thanks to the team at MyGC for the opportunity to have a chat about the upcoming Australian Transplant Games.
Transplant Athlete High Performance Camp – the inspiration, hurt & fun….
21 Mar
Picture this – a sweltering Gold Coast afternoon, 25 individuals who have been to the brink and not only recovered – but are thriving examples of what organ and tissue donation, and a health focused life can be.
Last weekend, a very special event occurred and I was lucky enough to be part of it. As a first timer, my experience was no doubt different to those who have been there before, but I want to share with you some of the highlights.
In a strange twist of fate, I ended up emceeing the media conference and launch of the 2018 Australian Transplant Games, at the Super Sports Centre, Runaway Bay. This launch also marked the start of our 3-day High Performance Training Camp. The Queensland Government is a major supporter of the Transplant Games, to be held here on the Gold Coast September 30-October 6. Health Minister, The Hon. Dr Steven Miles spoke of how this event would increase awareness and hopefully an upward swing in organ and tissue donation.
Following the official proceedings, we split into our respective sports and hit the track or pool. That first session under the guidance of Coach Stephen Howell was the most alive I have felt in years. Although I’ve been back in the water for a while, the challenge and absolute thrill of having a go really got my heart pumping! I sucked in some big breaths with each lap and as I smashed the wall at either end of the pool, I looked around and thought about my fellow transplant athletes. While my body and its organs, is now running on someone else’s stem cells, some of them had someone else’s heart or lungs helping them reach the end of the pool. Whoa……. I said some silent, but powerful thanks to our donors, their families and our medical teams. The emotions were running high, but while there was a little rest between sets, there wasn’t too much time to lose focus. While Steve pushed us hard, he also had us laughing. Like when he nicknamed young Logan ‘donkey’, as a term of endearment. Steve explained that when he saw real potential in a swimmer he’d ride them like the last donkey in town. Nuff said.
We enjoyed team meals in the dining hall, surrounded by international athletes in town preparing for the upcoming Commonwealth Games (including the Indian basketballers like ‘One in a Billion’ Satnam Singh! who graciously posed for a pic and hilariously high-fived/low-fived me when we passed between our rooms and training sessions:-). The vibe was sensational. The conversation covered everything from heartbreaking transplant wait-list experiences, to inspirational tales of recovery and determination to really live (like they say, ‘no-one lives like the dying’). I wished I could bottle this. Not just for my darker moments, but for anyone who might find themselves needing a little light at the end of the proverbial tunnel.
My ‘body scans’ went from analysing the pain, its severity and what medication I could take to try and control it, to how my muscles were feeling having worked harder than they had in a long, long time. I doubted whether I could keep up, but despite the hurt and exhaustion, was set on living up to the hashtag I started using during my transplant #stillkickin. In this case, I literally was still kicking!!
We were imbued with knowledge from experts during Strength and Conditioning (Adsy Gordon), Nutrition (Travis Ronaldson) and Sports Psychology (Craig Pearman) sessions. A lot of us struggle with fatigue just getting through the day, so this lecture format side of things was at times, quite tiring. The information though – so beneficial.
A key point of discussion was Internal and External motivation. A room full of people who have survived, and are thriving after transplant, perhaps don’t need to be taught about internal motivation. Without it, we all may have rolled over, given up, quit. It’s that beautiful combination of internal and external motivation that has created success. I heard so many stories of athletes not wanting to let their family, donor family or Dr’s down. It’s a powerful mix.
Speaking of power…we were gifted a very special insight into world class competitive swimming, with visionary of the sport, Bill Sweetenham. As a mad-keen young swimmer I watched some of his pupils including Tracey Wickham, power to glory on the Olympic stage. Bill’s name is synonymous with some of the most successful international teams in history. I was shaking like a leaf when I entered the ‘Elite Room’ and reached out to shake the hand of greatness. There he sat, in an empty room, just his big hat and dark sunnies and a bucketload of stories to share. I could listen for the rest of my days, but we soon found our way to the pool deck. Holy hell. I was so bloody nervous to strip down to my togs and hop in, I had to go and tell him I was terrified! All of a sudden my head had forgotten how to swim. As Bill took a seat laneside, we all slowly settled into our groove. Before too long, he had us all lined up, hanging onto the side of the pool listening intently to little tweaks we could each make. Teenage transplant recipient Claudia was given the somewhat unenviable task of jumping out to demonstrate getting full reach from a stroke. Whilst manipulating body position in that way, in front of all of us may have been daunting – Claude handled it like a pro, and I winked at her Mum Anna saying “she’ll never forget this.” None of us will.
Bill generously shared more stories with us (as we recovered from a session in the ice baths – another first for some of us!), he detailed the importance of balance and fun. What a way to cap off an unbelievable afternoon!
Some participants opted to sleep in on the final morning (totally cool given the workload and long days), while others managed a final hit out. I’m happy to say that although my body was screaming with pain – it was great pain – and I was in the water by 6 am. The mental chatter was strong, but there was no way I was missing this last opportunity. Apart from Coach Stephen giving us drills we could test, then take away, he’d also built enough confidence in our group to critique each other. The kindness and positive feedback was palpable. How all of us will grow as a result. I am so excited for the Games!
I grew up swimming, enjoyed training and loved to compete. I can’t say I ever had fun in the water though. That said, it is my ‘happy place’. I can float on my back for hours. Having been hooked up to machines to keep me alive, I revel in the freedom. The cold rush as I dive in, the swoosh of the water passing my ears, the exhilaration I feel powering along the black line and the absolutely life-affirming satisfaction at hitting the wall. Fun though? Nope, not really. Until the other day. The last few minutes of our swim session, Coach Steve suggested a Michael Phelps drill for vertical kick training (you’ve gotta watch this!). Ahhhh, yeah, right. Well, getting out into the middle of a lane, dropping till your feet are flat on the bottom, then squatting, pushing up, streamlining and butterfly kicking up out of the water like a rocket is unreal! Such an incredible feeling. And yes, I had FUN!
The reality of organ and tissue donation is very simple – people that were once terminally ill, are now here.
CEO of Transplant Australia, Chris Thomas provided this example at the launch of the Games and start of the High Performance Camp, going around the group asking ‘years since transplant?’ In a staggering display, we added up the numbers and we, those of us gathered who had been granted this precious gift, have so far enjoyed an additional 266 years of life. That is a whole lotta birthdays, anniversaries, children and other milestones that may not have been.
Although the post-transplant life is very much filled with medical appointments, medication and a multitude of side-effects, it is life. Life that, if not for our donors, we could not sustain. I feel strongly it is my duty to honour my anonymous donor and my team, by looking after this body post-transplant, and live the best life I possibly can. Thank you, may never be enough.
I encourage anyone reading this, who hasn’t had the conversation about organ and tissue donation with their loved ones, to please do so. Your decision can and will save lives.
Make the decision count – donatelife.gov.au
Huge thanks to Nick Farley for some of the above images. Check out the rest of the HPC via his Insta farleyphotographix
Better out than in…
4 Jan
This body is so capable – but it’s been through enough.
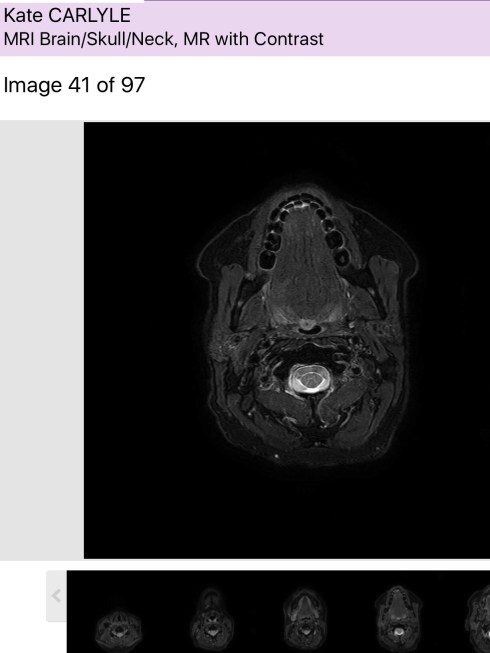
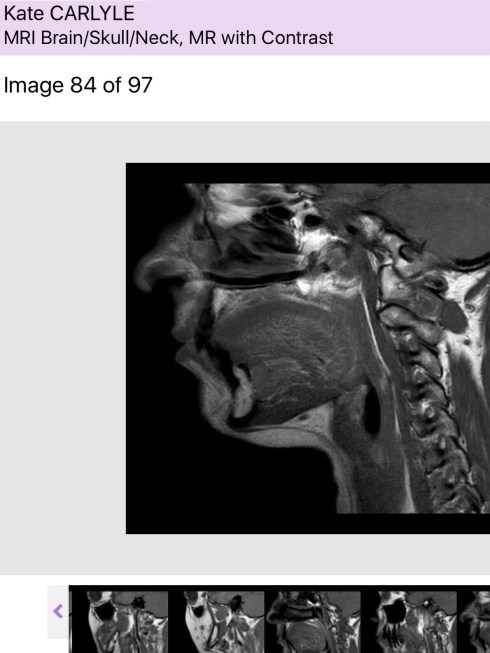
I truly believe that, which is why I’m not completely terrified of a ‘suspicious mass’ recently discovered in my mouth.
It’s coming out in a few days time. The surgeon is highly experienced and during the necessary scans and tests of late has become a good fit in my (now rather extensive) care team.
Whilst acknowledging if this case were for his surgical exam, he would leave things for a few months, he duly pointed out that this is real life and this patient has a nasty cancer history. So, we agreed that after observing for a set period – the ‘watch and wait’ approach is clearly not in my best interests.
This may turn out to be a sublingual gland that is just ‘misbehaving’ given my overall health. Fingers crossed. If it is however, another hit of the ‘Big C’, I’ll deal with it as I have the last three.
Fortunately they won’t have to go through my face (or brain! I was shocked when he mentioned casually that sometimes that is the best/only way to get to the area), they’ll go into the floor of my mouth, through my mouth.
My gut feel on this one is that it’s okay. Another little curve ball if you like. My instinct has never let me down before, so let’s hope it’s still on point.
Fights don’t have to be loud…
29 OctSometimes the most difficult battles require a peaceful, gentle focus.
A huge shoutout to my Mum and friends Nerida, Lina and Ian for letting me have this lately while I’ve been unwell. Sincere apologies to everyone I’ve unintentionally snubbed. Please know when I say I’m ‘average’ or ‘not the best’, I’m not just looking for an excuse to get out of life. It is quite often, quite serious.
There’s definitely a pattern to my immune system taking a dive. Sometimes it begins with a fever, other times my skin becomes insanely itchy and a horrible blotchy mess as the Graft Versus Host Disease rears its ugly head. I sleep a helluva lot and heavily (to the point where Mum routinely checks to see if I’m breathing). My body is in pain, struggling under the stress of just the basic functions. During a recent 4-5 day stint, I was reduced to sliding out of bed onto the floor and crawling to the bathroom (much to the delight of Lila and Phoenix – who thought it was playtime for puppies!), my bones just couldn’t stand my own body weight. I fevered, had the shakes, vomited violently, sucked on Hydralite ice blocks to try and get some fluid in….I tossed and turned, writhing around with a relentless pain as my head pounded so hard the pressure on my eyes had me believing it just may be possible that they could actually shoot out of my face!
It would’ve been a whole lot easier to just send me back to hospital. There’s been calls for the house doctor, the ambulance and a couple of readmissions. I want you to understand my reluctance to go.
I’ve lost count of the surgeries, procedures and treatment over three rounds of cancer and Bone Marrow Transplant. I’m only just starting to realise though the deepest scars have been caused by my extended period in isolation, while fighting for my life.
That tiny room, with my bed, a chair (for my limited visitor or me on a good day) and ohhh those beeping machines (helping to keep me alive). It was another world – where the window didn’t open, the temperature didn’t fluctuate and when not being fed ‘hospital food’ my GI tract was so fried I was being nourished through a tube (sometimes more appealing than what the kitchen was dishing up).
As I try to adjust to my new body and life ‘outside’, that experience is still haunting. After being ‘away’ for so long, I truly crave being in social situations (and have seriously enjoyed some special events like weddings, live music, meals out and art exhibitions – including Dior;-), but they test me on every level. This can not be compared to our war heroes, or those who suffer from other causes of Post Traumatic Stress Disorder – but I am terribly affected by colours, noises, smells and just general activity. Fending off panic attacks is not something I thought I’d be faced with, having dealt with the Big C!
Some of my bones have packed it in, others are following. The hip that’s been replaced is good. The other one, not so. With the help of my team and pain relief, I’m now walking unaided! Re-learning how to walk and drive are big things. It’s almost easy to forget I’ve had to retrain in the smallest things, such as writing. At times I am so clumsy with dropping everything I pick up I wonder how on earth I’m going to get on with life. Despite the toll, I know that with work, the weakness will make way for strength.
I have developed a reliance on heavy duty painkillers such as Morphine and Fentanyl just to keep on top of excruciating pain. The bone-crushing pain is constant and most intense at night. It drives me to tears. The best way to deal with it, is to not let it get out of hand, by keeping Panadol running underneath, a patch of Fentanyl providing dosage across the board and Ordine (liquid Morphine) or Fentanyl lozenges for breakthrough pain. Not exactly the way I want to live, but the alternative is even more debilitating than the space cadet impact of opioids. This situation though, leads to frequent questions and discussions about addiction to such drugs. A bit of a bind to say the least. I’m doing the best I can.
Emotionally, I’ve got a lot to work through – how I’ve dodged a bullet again, how it is I’m alive while others who had so much to live for have succumbed, the changes to my body, the incredible impact these illnesses and treatment have had on all areas of my life, how I needed (and luckily received) stem cells from an anonymous donor when my own sister was a match and had committed to donating, reflecting on how my usually supportive husband gave up on my fight and walked away – completely (might as well have left me for dead), and trying to settle into life with all my worldly possessions in storage while I’m staying at Mum’s. The beauty of that is we genuinely enjoy each other’s company, help each other out, our four-legged fur babies are well looked after and the general vibe is always pretty good. I still very much live with the ‘no negativity allowed’ sign on the door!
When I’m okay – I’m really okay! However this post-transplant life continues to throw curve balls. Whilst trying to save you the horrible detail, know that the challenges I face with getting this body to work well (or even remotely like it used to), is dependent on so many factors – including the nature of my anonymous donor bone marrow transplant, complications including GVHD and the raft of life-sustaining anti-rejection medication I take daily. Those drugs (which I have a love/hate relationship with!) have had an enormous impact on my life. Day-to-day can be tough. Ensuring I can get the meds in, tolerate food etc. is quite exhausting. So, when doses change, the adjustment can be fierce. When my immune system falters, it can be incredibly nerve-wracking.
Everyone knows how grateful I am to those gems in my care team – the Drs’ and nurses, but I just don’t want to see them too often! Staying out of hospital is the name of the game.
Quiet time can sometimes be the hardest.
Tap, tap, tap.
17 OctI’ve decided to stop blogging.
Well – truth is I’ve been so slack at it since my Bone Marrow Transplant, I feel guilty. Reaching this decision really just comes down to facing the fact I’ve been doing a pretty average job at it.
I’m lagging behind with writing about so many things like the Pink Polar Expedition (in support of the McGrath Foundation), speaking at Red Cross events for National Blood Donor Awareness Week, the truly tragic death of my former ‘roomie’ less than three weeks after her BMT, surviving my first cold, re-connecting with friends and family and trying to find the ‘new normal’ following such a long stint in isolation and several near-death experiences… ‘Looking’ better, but feeling decidedly wretched, being abandoned by my husband and feeling loved and welcomed by new friends. Ohh, then there are the ‘quality of life’ issues which present themselves on a daily basis.
There are numerous reasons I’ve been so neglectful of my blog – the main one of course is that I’ve just been too sick. I know technology is great and can make it easier, but honestly – some days – just thinking straight and getting my thoughts ordered enough to make sense, is a battle. I am so scattered and at times wonder if I’m totally bonkers with the things that fill my brain. Let’s just say my headspace has been rather cluttered with arguably some of life’s big ticket items.
Seriously though, I am feeling perhaps this medium has run its course. Not across the board, but for being the most appropriate outlet to share ‘my story’. I even hate the way that sounds. So presumptuous. Like you must want listen to what I have to say:-/
On some levels, what I’ve shared on this blog is deeply personal (gory pics and all), yet on others – it has barely scratched the surface.
During the harrowing ordeal that was my Bone Marrow Transplant, my Mum helped keep those interested up-to-date with my situation using various social media channels. They’re a rather effective way of providing a snapshot. (When my eyesight was so poor I could hardly see, she typed. When I was unable to speak, we found a way to communicate and she continued to share.) SM has a place – a pic/comment here and there and I will keep it up – but it’s hardly a comprehensive record.
I had fully intended to go back to blogging, as I had throughout my breast cancer experiences. But, apart from the cognitive decline and difficulties I encounter with fatigue, there are still a great many side-effects of this transplant, treatment and medications that leave me struggling.
At the same time, as I try to get back on my feet (pun totally intended given my dodgy hip situation!) I am regularly asked to share my ‘story of survival’. Whenever there’s a request and it is possible I will do this for awareness campaigns, charity events and motivational opportunities. I feel very strongly about using these experiences for good, in the hope that someone – just one person will benefit, in some small way.
Perhaps though, I could (and maybe should), use the time and energy I have left, to write a more in-depth account? (let’s face it – there are not many of us with such an ‘interesting’ medical history still around to tell their tale). There are times I feel compelled to document some of these experiences, so others who are facing or are involved in similar situations may find some help, hope or solace.
I have never written a book. Hell – I wrote and presented radio news three-liners for a living!! I don’t even know how to begin. My first thought is to ask those who’ve paid a bit of attention over the years and who may be potential readers, what is it you want to know? And if you don’t mind indulging me – why?
..before you go!
21 Feb
As keen as I am to get home later today, I knew it would be foolish to rush. One of the benefits of not pushing, is that final checks revealed my haemaglobin has dropped since the surgery (as was expected.)
So, I was able to have a last minute blood transfusion to ‘top me up’. Thank you again you wonderful donors out there, still a year post transplant- my health is being improved by your generosity!

The ‘To-do’ list at Discharge includes a final physiotherapy session on the ward, confirming future appointments with Orthopaedic specialist at ‘complicated fractures clinic’ and of course with my BMT Consultant.
I must say I’m looking forward to a big bowl of green Asian veg, with sesame oil and soy sauce. The hospital fare wasn’t really doing it for me and I found myself humming ‘….hospital food’s gettin me dooooo-owwnnn’ ah la David Gray.
Tell me you don’t find this ‘Moroccan style chicken’ appetising?
(I promise, in that ahhhhh, slop, there is one piece of chicken! Look closer. It’s down there on the bottom right of the plate!)
Final step was to change the dressing on my surgical wound. Nurse Jaynne – who’s heading for a career in the ADF, did a great job getting this scar across my thigh and butt looking clean and ready to go home.

Puppy cuddles await…
21 Feb
There’s nothing like home. Sure, you can think instantly of the creature comforts such as your own bed, a nice lounge, the ability to be able to grab something from the fridge when you like etc. but for me – the things I’ve missed most are of course my puppies; Ch’i, Lila and Phoenix Hope.
Paul is doing a great job looking after them, but we both are so grateful to our darling friend Krissy, who is again going above and beyond. This crazy, loveable lady goes to visit our girls everyday. She hangs out with them, cuddles, plays and just keeps them company. A beautiful extension of our friendship is how seriously she takes her role of ‘Godmother’ to the girls.
This is a special pic, as Krissy really doesn’t like having her photo taken.
…and not to be left out, my little brother Skype’s in to see I’m ‘following Drs’ orders’. Crack in’ day in Adelaide – look at the colour of that sky!
THR – done.
20 Feb
Once again, I don’t fit into the ‘typical’ profile of a patient requiring this latest treatment – a Total Hip Replacement (THR). Nothing I can do about it, but a little more detailed planning for my various medical teams.
Clearly the Bone Marrow Transplant team, led by Dr Kennedy are my ‘go-to’ guys (& girls). This Avascular Necrosis of the hip and THR is being handled by Orthopaedics though, so there’s a whole new team and dynamic to consider. Let’s just say it’s been interesting….
The Australian Pain Management Service (APMS) is heavily involved! As is the Physiotherapy team. Include the nurses and you’ll understand I’m never lonely – hospital is a very busy place and I see a lot of people! (Usually right when the heavy drugs are kicking in and I can’t string two words together!)
Thankfully today I had a fun visit from one of my ‘besties’, from way back in high school days. She’s seen me indulge in too many champagne’s so is pretty understanding. Today though, Jen; a very capable mother-of-two, took over bathing duties for me! As she gently washed my back, I giggled so hard I was sure I was going to fall through the seatless toilet/shower chair I was perched on! Not your average hospital visit🙈
Thankfully my drain hasn’t been collecting that much blood, so it’s coming out! One less tube….
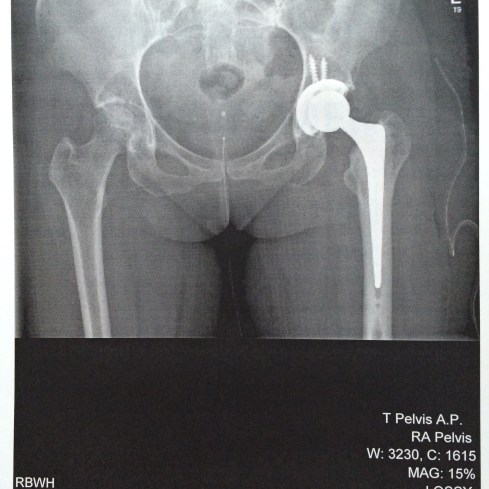
And this my friends, is my new left hip!
Incredible isn’t it?
This x-ray also shows a deterioration of the bone in my right hip, in line with the early stage Avascular Necrosis reported in the MRI a few weeks back.
Everybody shufflin!
20 Feb
Day One and I’m proudly ON MY FEET WALKING! (Okay shufflin’ – but I’m fully weight-bearing with the slight aid of a rollator. UNREAL!
Mum had just arrived – how cool!
Dr Halliday earlier confirmed operation went well and that it would be only be a short stay in hospital.
When I asked about doing the other side he replied, “I’m not going to hack into your right hip, it really doesn’t look that bad. I don’t know why you’ve got this pain.”
Well, I thought we’d been over the fact that crumbling bone might have something to do with it, but he now seems unconvinced!
He told me that when the cartilage was peeled back, it revealed a mass of crumbling, almost powdery bone-like substance and that the deteriorated bone had basically been ‘encapsulated’ within that cartilage. There’s no saying that’s not already happening to the other side.
That’s the report from the initial MRI, we’ll see how I recover from this THR and whether there’s been any progression of disease in the right side.
Can SO do this..
19 Feb
This is hard core. I’m trying to recall some of the conversations and incidents pertaining to my care and the expected success of this surgery on my left hip (keeping in mind the right will have to be done soon).
Whilst ‘mechanically’, it’s pretty standard, the finer details in planning and taking necessary precautions have involved a lot of people with expertise in several key areas. It’s not solely an ‘Orthopaedic job’ nor is it ‘Haematology’, however big decisions to make this as safe as possible require specialists from both fields.
Apart from my Coke ‘splash’ yesterday, the team set-up a platelet transfusion for me to cover two hours of surgery time + an additional bag. (They have to be agitated, so I willingly took on the role of ‘chief agitator’😜, while I would otherwise have been just laying around watching someone else do it.)
It was a big bag too – 340mls.
The Anaesthetic and pain relief was a bit tricky for the team to fine-tune, given my allergies (I can rattle them off quickly now – Codeine, Tramal, Endone, Ketamine and Erythromicin!!)
In Pre-Op, my surgeon said he wasn’t worried about fixing my hip, but was concious of my ‘overall poor health’. A seemingly simple little issue could become a life-threatening emergency for me very quickly. Still, my hips are dead/dying and the left one is broken – this has to be done. Happily, my neutrophils are good and the infection risk is being handled as well as humanly possible.
Food (with GVHD considerations), fluid, oxygen are other elements being taken into account.
My drug-affected recollection is that I tried to smile the whole way through, even when sliding across onto the operating table. It was very noisy when I drifted off to sleep; metallic banging of instruments, people buzzing around and the Anaesthetist holding my hand firmly. We had discussed doing a nerve block in both hips, so I could enjoy 8-10 hours of reduced pain. The surgeon had agreed and I said thank you before 💤💤
NASTY – but alive and I’m in one piece. Those were my initial thoughts on waking.
Navigating my way through the next crucial 24-48 hours is not going to be fun, but I have always found that by being observant, focused and actively involved in my health care, things can be easier.
The nurses here in Orthopaedics don’t know me as well as the guys and gals in the BMT unit. It took a bit of persuading to make them see I was ready to get up on the day of my surgery…hey, if an 80 yr-old can do it, I can do it!
WOW….. Breath-taking. I remain still, politely ignoring others in the room while I allow myself to soak-in the beauty and power. This simple sequence, which has today led to me being on my own two feet (relatively pain free), is awesome. Life is….awesome.
Morpheine with Coke chaser = surgery delay!
18 Feb
Oral morpheine, my go-to pain relief at present, tastes pretty awful. This morning at the unsociable hour of 4am, I decided to wash it down with a mouthful of Coke.
Dumb idea.
As the lovely Nurse Zach and delightful Dr Tom prepared me for surgery, with blood tests and platelet transfusion etc. they casually asked about the last time I ate or drank. I confessed to my post-transplant sweet tooth gulp of the ‘black aspirin’ that followed the morpheine and other meds, and they just glared at each other.
Although I was safely within the 5am cutoff time for fasting, Coke wasn’t water or black coffee or cordial which were all permitted beverages. Their faces told me I was in trouble…So much trouble the Anaesthetist came and changed the surgical list. I’d been bumped from position of first cab off the rank.
Now, I sit, I wait. I am grumpy, with a dehydration-related blinding headache. Don’t suppose they’d give me a can of Coke? A sip?
Hammer time
18 FebJust think for a second about using a power saw to cut out a significant chunk of your skeleton…. There’s nothing delicate about today’s total hip replacement (THR) surgery.
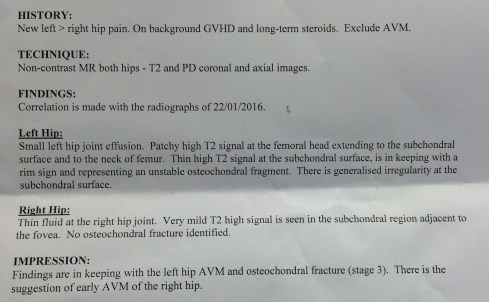
Sadly, my hips are in bad shape following my bone marrow transplant and long-term steroid use. Both have a degree of Avascular Necrosis. The left one (being tackled today), is fractured across the head of the femur.
I’m tired, in serious pain and feeling rather impatient to get this done. It’s hot, I’ve been fasting, I’m thirsty!
Enough of the whinging already, let’s get this done…….
Home – but not as I know it.
18 Feb….And not for too long.
I know this is only a short stay, under two weeks to enjoy the comforts of home and my gorgeous girls Ch’i, Lila and Phoenix Hope (any excuse for more puppy pics!)
After assessment by Physio and Occupational Therapists, I’m out of hospital with crutches, rather than a wheelchair, rollator or walker.
Good thing hadn’t planned anything else in the time back on the Coast, as I have been unexpectedly sick. Unwell to the point where I actually packed my bag for hospital expecting to be re-admitted. I didn’t feel sick, but all of a sudden was violently ill, repeatedly – for no obvious reason. I had one 24-hour period that is a complete blur of tumbling out of bed to the bathroom, having a ‘few moments’, before crawling back to bed in such a state I could barely believe it. I was heaving nothing, unable to keep a tiny bit of water or electrolytes down (let alone all the medication I have to take) and shaking uncontrollably. Completely exhausted, I willed the day and night to end, so I could catch my breath!
Which brings me to breathing. Ohh such a simple, critical and beautiful life-sustaining act. Countless times, people have asked how I keep getting back up for the next round of ‘misfortune’ I’ve been dealt. To be completely honest with you, more often than not it comes down to just breathing my way through. My daily yoga practice (sadly somewhat altered and less-energetic of late) is my most effective coping strategy (okay – that and a slightly warped sense of humour!) How do I not get completely overwhelmed, lose my cool, or drop my bundle? By choosing to be ‘mindful’ at every opportunity. The term ‘mindfulness’ is quite en vogue, but it’s really just a modern way of describing a behaviour that through the ages and practices such as yoga, Tai Chi and meditation, can be put simply as ‘focusing on the moment’. All sounds a bit ‘new age’ to some, but it’s historical roots can’t be denied. I’m so grateful for my Nana’s influence here. As very young children she taught us (and thousands of others who attended her yoga classes), to breathe, focus our thoughts, be calm in the decision making process and….breathe. My deep affinity with this learned behaviour is something that I have continued to seek out in adult life through readings, classes and courses. It is most definitely a skill, an incredibly valuable one that has helped me navigate some pretty tough challenges. Don’t get me wrong – the odd meltdown still occurs, but is usually rather mild and short-lived.
This ‘hip drama’ has pushed me almost to my limit. I can’t quite put my finger on why though. Perhaps it’s a combination of the timing around my 1st birthday (on which all I wanted to do was celebrate being alive!) and the break-up of my marriage, the physical incapacity, loss of recently regained independence, turmoil of major surgery and all that entails (twice over!)…..not to gloss over the PAIN. My goodness, the intense bone-crushing pain, the searing nerve pain, the all-over hurt my body is experiencing is unrelenting. I’m on a cocktail of pain relief medication courtesy of the Palliative Care and Pain Management experts. Keeping on top of it is so tiring and the drugs are not without their own side-effects. As Pink once sang “……morpheine is making me itch!”
Soon, I’ll have a new left hip, made from a combination of steel, ceramic and plastic. Soon after that surgery, the team will do it all again for my right side.
Time to get back on my feet.
But ‘I’m’ the patient.
5 Feb
9pm tonight, almost exactly 48 hours after that horrible experience with my ‘roomie’, Boom! Another.
A voice from behind the curtain demands “nurse get me a sleeping tablet – you’re keeping me awake!” “I’m sorry, what can I help you with?” She asks.
“You, because of you I can’t sleep, you’re in here socialising!” She spat. The nurse replied “Ahhh, well no. It’s part of patient care to develop relationships and yes, we have been chatting.” When challenged again, the nurse pointed out it wasn’t that late and it wasn’t unreasonable…also that the patient still had her TV on. “Yes – and it’s LOUD!” She bit back, “to drown out you and Kate.”
What?! She knew my name and used it?!
“Excuse me”, I said “after the other night, this is intolerable.”
She exclaimed at the top of her voice, “but I’M the patient!”
I took a deep breath, but couldn’t help myself, eventually saying “I guess I could politely point out that I am too”. As the nurse reminded us that we had to share the room, I painfully shuffled my butt to the edge of the bed to lean over and reach my new crutches. I went to leave and for the first time saw the lady behind the curtain. I was in complete disbelief that someone could be so unwell, yet find the energy to be so aggressive. As our nurse left, the nurse in charge promptly entered to try and break it up. In a frustrated hobble to the door, I thought to myself, you lady are a seriously nasty piece of work.
Over the past few days I have learned that sadly, her condition is terminal. I am acutely aware of the range of emotions she may be experiencing, fear the one I have overheard her talking about the most. It makes me upset that she appears to be leading such a miserable existence and that her final weeks or months are scarred by this sort of outburst.
As the nurse in charge tried to calm the situation, the woman piped up at me again “You have influence in here…” What?! I said “I beg your pardon?” She raised her voice even louder, “Ohhh don’t say what, I know what I need to say and I’ll do it in the morning….”
This was bullshit. I was out. Unsteady on my feet, I gently swung my broken hip forward and put one leg, then one crutch in front of the other and went to the patient lounge.
Deep in thought over the awful confrontation, and trying to reason that everyone deals with stress differently, I burst into tears when the nurse in charge came in to make sure I was okay. I was shaking.
As I apologised, saying I felt sorry for the nurse looking after us and that I should have left the room without saying anything, the nurse in charge told me she was glad I stuck up for myself. She consoled me with a tub of lime jelly and shared with me some horror stories of abuse and violence from other times in her nursing career. Truly shocking. I now know why there are signs in health care facilities all over saying things like ‘zero tolerance’.

I realised I couldn’t sleep in the lounge and was not looking forward to lying on the other side of the curtain to someone I’m so repelled by. I imagine it might be like being on school camp and having to share a tent or dorm with the class bully.
News travels fast and the rest of the nurses on duty were on it. Many asking if I was alright as my crutches and I slowly clunked our way back to the room.
As I sit here typing away, I’m not so concerned about the tap-tap-tap of my fingers on the keyboard. The smart-arse part of me is tempted to turn the TV on, and crank the volume!
Lights out!
3 Feb
I can not believe this just happened.
My ‘neighbour’, the woman in the bed next door in this 2-bay room has picked a fight with me about having the light above my bed on.
A bit miffed, I asked her if she was actually asking me to turn it off? (It was 9.20pm). I told her I was waiting for assistance to get to the bathroom (’cause I can’t walk!) and I would switch it off when I came back. I went to the bathroom, had a sook with the nurses and returned, pulling her curtains closed as I shuffled past on my roller/walker thing. I turned off the overhead light, but before my machines were even plugged back in, she went on the attack again.
The light she was now angry about was on the machines providing me with drugs including pain relief!!
Incredulous, I hit the call button for the nurses. As one entered, I stifled tears as this woman told me she ‘couldn’t possibly sleep with the light on, she was in pain and had such-and-such disease.’ This was obscene. All I could say was ‘do you really want to go there?!’ I covered my head with a pillow as the nurse calmly explained it was a share room, don’t fight, we had to try and get on etc. etc.
She’d had her TV blaring all afternoon, while I had visitors…. No-one complained. Clearly we are both sick, otherwise we wouldn’t be in here.
As I appealed for a little more respect due to that obvious fact, the nurse exited and my neighbour promptly started snoring!
Sweet dreams💤

Complications and conversations.
2 Feb‘Cranky-Pants Carlyle’ is a nickname given to me by a Program Director I used to work with in radio. As News Director, I was tough, didn’t tolerate inaccuracy and encouraged, no demanded the highest of standards. One station’s Managing Director used to introduce me as the ND who had an iron fist in a velvet glove. I was just doing my job and expected the journalists in my newsroom to also do their best. It was a privilege to report the news everyday, we had to get it right.
You know how amazing my medical care has been. Tonight though, I’m a little disappointed. Without going into too much detail, bagging anyone or getting anyone into trouble – I feel a bit let down by ‘the system’. Certain individuals have worked very, very hard, have gone above-and-beyond to get scans done and resolve this latest complication. For this, I am very grateful. In the meantime though, I feel as though I’m going backwards.
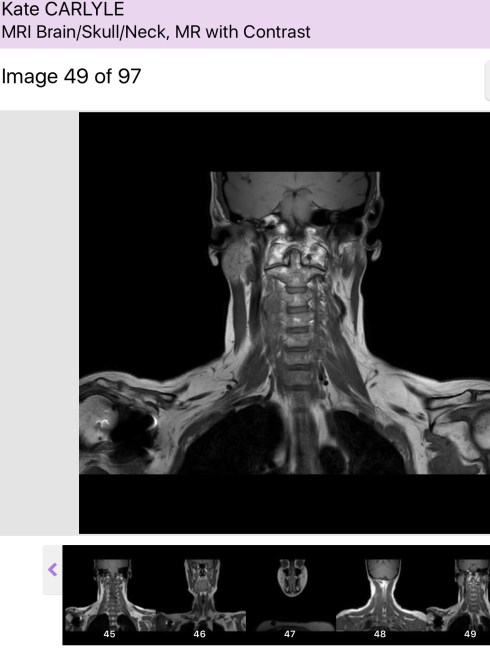
I came to hospital last week for an MRI on my hips and then to have my 1 year from transplant Bone Marrow Biopsy. I was awoken by Dr Kennedy to tell me I had Avascular Necrosis of both hips and also a fracture in my left hip. Nasty. I wasn’t going home anytime soon and was not allowed to put any weight on my fragile/broken joints.
Thankfully I was admitted to my old ‘home ward’ of 5C, where the familiar faces were as friendly as ever. The nurses did everything in their power to make me comfortable. Lying around is not something I’m keen to do after spending so long doing just that before, during and after transplant. (It’s also a real kick in the teeth for someone just starting to regain her independence.) All of a sudden, I wasn’t allowed to drive, couldn’t go home and was not able to see my beautiful girls!
I’ve worked so bloody hard to get back on my feet, but now I’m being forced to put them up.
While the nurses keep the medication for pain coming, I’m awaiting a consultation with the Orthopaedic team on what should be done with my hips. I’m waiting patiently. The Physiotherapist has been to discuss the use of a wheelchair, walker or walking stick both before and after surgery, we also talked about the prospect of doing one surgery on both hips or having them operated on separately. An Occupational Therapist came to talk about how I would look after myself at home, living on my own, with three dogs and still needing to get to a heap of medical appointments. They are going to send someone to do an assessment on things like access, my sleeping arrangements, the bathrooms and kitchen.
What I’m needing now is a game plan and only the ‘Orthopods’ are suitable experts, everyone else is sweating on their advice and action.
To say I’m a little frustrated is an understatement. Keeping this in-check is hard, especially when I’m in such extreme pain. The flip-side is I have been totally overwhelmed by the people who have ‘shown up’ during this tricky time.
A group of sensational women I went to high school with 20+ years ago have been right with me in the thick of this – bringing cheeseburgers and Doughnut Time doughnuts and a nightie for when I have the op/s. My amazing neighbours came armed with delicate tea, lip balm and moisturisers – as well as a GP’s caring and understanding. The true blessing though is a precious friendship. And a Kindle loaded with dozens of books was hand-delivered all the way from the Gold Coast, by another special friend. This was so thoughtful and such a lovely surprise!
I’ve become such good mates with some of my medicos. So cool. The co-ordinator of one of the Clinical Trials I’m in collected the last lot of bloods for research – but has again offered an ear should I need someone to listen. Many of the other nurses have kept me entertained in the middle of the night chatting about everything from some of my transplant horror stories to little Phoenix, favourite restaurants, music, weddings and babies. There’s never a dull moment, in fact there’s been a revolving door. Good thing I love a good story!
New Wheels
30 Jan
No….it’s not a new car, I am under strict orders to keep off my feet.
Not only do I have Avascular Necrosis of both hips, my left one is BROKEN! I’ve been walking (awkwardly shuffling) around on a broken hip and am lucky the other hasn’t also disintegrated.

I didn’t get to go home from hospital yesterday and will most likely be in for a while as I need hip replacement. The Orthapaedic team is due to visit today.
Please enjoy Dr Kennedy’s doodles;
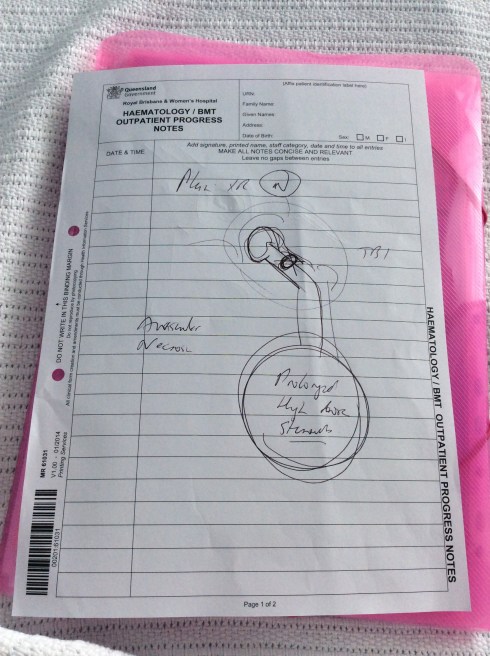
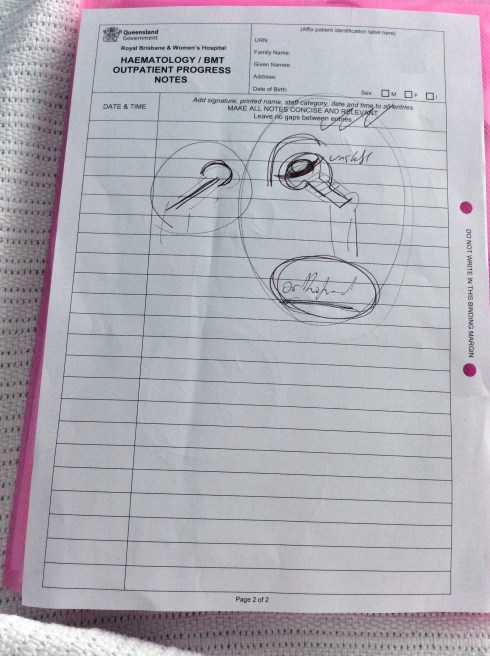
I’m gladly accepting some heavy duty pain relief (well I know what’s causing the excruciating pain now!), have a few stitches in my right arm after having a spot removed by the Dermatology team during checks, have a cannula in (as I no longer have a central line) and have a very sore back/butt/hip on the right, where the Bone Marrow Biopsy was performed yesterday. Body is a bit of a wreck.
In the meantime, I’m very pleased to say I’m back in the familiar surrounds of 5C, with so many of the special nurses that looked after me during transplant. We shared chocolates yesterday as we marked my 1st birthday, or ‘cell-iversary’ together.
What a wild ride!
Granny Hips
23 JanI think I did pretty well to get out of hospital without three things; a wheelchair, walker, or walking stick. Although weak, I was determined to shuffle along on my own two feet no matter how long it took to get to my destination.
Recently, I’ve been struggling to walk and could’ve done with the aid of any of the above! Yep, I feel like a bit of a Granny.
A crushing, searing bone pain has really been affecting my hips – particularly the left one. It’s an un-nervingly familiar pain. Not an arthritic kind of ache – a definite, stabbing pain deep into the joint. I say familiar, because along with fatigue and unexplained bruising, this bone pain was the first sign of my MDS which quickly turned into Leukaemia. Before we knew what it was I was being treated by a Rheumatologist who thought my bones were sore from my previous chemotherapy and gave me cortisone injections to try and ease the pain. No amount of steroids were going to help!
My next Bone Marrow Biopsy, which will show any worrisome activity, is a week away. Until the results are back, I’m choosing just to enjoy every single day. With no anxiety, stress or panic. As I’ve said many times before – I can not control this, but I can control how I deal with it.
Poor results from the BMB is worst case scenario. Next in line is Avascular Necrosis of the hip/s. In layman terms, the blood supply to the bone is affected and the bone dies.
I had an X-Ray yesterday showing my hips look okay. Apparently that’s entirely possible even when AVN is present. Both my GP and Haematological Oncologist suggested this might be my problem. Unfortunately, treatment includes a total hip replacement. I’m having an MRI in coming days.
In sickness and in health..
10 SepI may have survived the transplant process, but sadly, the same can’t be said for my marriage.
After almost 14 years as husband and wife and 20 years together, Paul has decided it’s time to go – he can no longer be part of this ‘world of illness’. It’s been seven years and three rounds of a hellish cancer roller coaster, a ride that he never asked to take. You can’t blame him really.
Paul dropped the bombshell about three weeks ago and I’ve been trying to get over the shock since. After a morning of me throwing up violently, he finally broke and suggested that if I want to ‘run away to become a monk with the time I had left, then he wouldn’t stop me.’ I was admitted to hospital that afternoon and later that evening came the explosion and shrapnel wounds…
My central line was hooked up to a variety of supportive therapies; fluid, pain relief etc. I lay in my hospital bed while we Skyped, and not long into the conversation Paul blurted out ‘it’s all getting too hard and if we split up then we can each just do what we want………..’ No judgement here about being so brutally open and honest – the timing on the other hand was dreadful. I guess there’s no ‘good’ time to drop something like this though.
So, I freely admit to asking for some additional pain relief in an effort to try and wipe me out from the nightmare unfolding around me. The big difference between the patient and everyone else is that others can choose to opt out – those of us with the disease can’t. Don’t try to tell me you understand.