It’s one of those stormy and unpredictable nights on the Gold Coast, eerie almost. Perhaps a reflection of my life at the moment as I consider that just as quickly as they roll in, storms fizzle out. Maybe the thunder and lightning are even Mother Nature’s way of reminding me that powerful, violent fury can and does end, often leaving a beautiful, fresh glow.
I do hope that’s the case with my current situation.
I must point out that I’m not caught up in a terrible bind, I’m just playing with words. However I do feel like I’ve been at the centre of my own ‘storm’ for a while now and quite frankly, I’d like it to pass.
In trying to bring about an end to a sort of stalemate with my marriage, I’ve decided to collect my two gorgeous girls and take up a room at my Mum’s place (okay – a room & bathroom + parts of her sewing room, kitchen, living, outside area….) Paul will move elsewhere and we will rent out the apartment for the time being.
Those of you who know me know how ‘house proud’ I am. More than that though, I truly adore living in this apartment. It’s in a great area, safe, quiet, in an amazing building, with brilliant design. It’s also a tad luxurious. This place is special for other reasons too. I think of it as kind of like an elegant NYC Brownstone – but white! The entry is through a glamorous lobby and we were lucky enough to secure one of the terrace apartments on the ground floor – so not only is there plenty of room for the girls, but there’s also direct street access. I can walk across the road to acres of parkland, the riverfront and the ‘magical tree’ I’m so drawn to, or pop over to the banks of the private lake. I also have a few neighbours I count as friends, who have become a big part of my life. It’s stunning in design, yet understated in its feel. The kitchen is just perfect for entertaining (which again, if you know me – you’ll know I love nothing more than having a house full of people to feed and clink glasses with), the bathrooms are fully tiled with beautiful travertine and I’ve decorated accordingly – continuing the earthiness with timber, leather and steel. We’ve added a really nice black granite circle of life water feature and the timber arbour is playing host to a very healthy wisteria. I am yet to see it flower in full bloom.
Elegant. Sophisticated. Home.
For the eight and-a-half months I was in Brisbane last year, I dreamed about this place. Every single day I willed myself stronger so I could return home. I can ‘make home’ anywhere, really. But this little apartment, well, it just feels good. I love everything about it. It’s the only home little Phoenix has known, where Lila loves to bail up the delivery guys and where my darling Ch’i took her final breath.
As much as I love this place, I’m not too naive to pin all my hopes on returning. I of course hope I will, but as we all know – a lot can happen in a short space of time. We’ll just have to wait and see.
There’s heartache and disbelief to deal with first. The reality has certainly been overwhelming these last few days, as I’ve moved some things to Mum’s, sold others and sent the rest to storage.
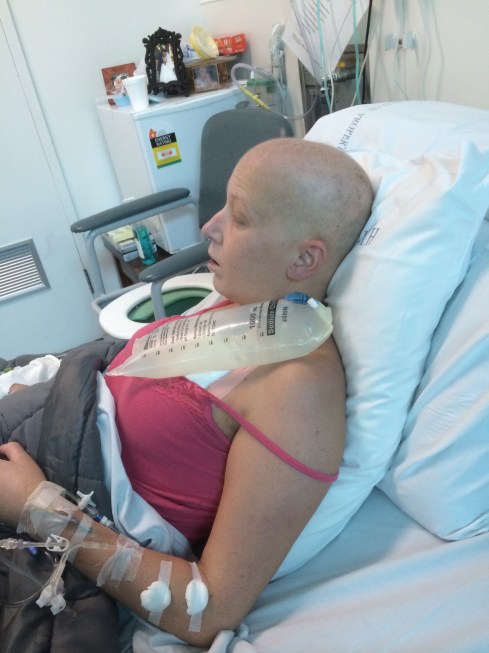
The emotions are running high. It’s devastating to be honest – but I need to try and keep everything in check. Seriously, the drama of three lots of cancer plus a bone marrow transplant isn’t enough? The destruction of my career, my marriage…and now this. I’ve had a gut full to be honest. What I could really do with is a break! This period I am certain, is meant to be THE most amazing, happy time of my life – as I should be celebrating the fact that I HAVE A LIFE! Courtesy of a lot of hard work by a great many people and of course, the generosity of my incredible donor. Instead, there’s more major upheaval as Paul leaves and blames the ‘cancer bubble’.
Well, fuck you cancer. I don’t need to be around those who can’t deal with you.
Fuck you cancer, I am a grateful soul.
FUCK you cancer, I wake up happy.