Picture this – a sweltering Gold Coast afternoon, 25 individuals who have been to the brink and not only recovered – but are thriving examples of what organ and tissue donation, and a health focused life can be.
Last weekend, a very special event occurred and I was lucky enough to be part of it. As a first timer, my experience was no doubt different to those who have been there before, but I want to share with you some of the highlights.
In a strange twist of fate, I ended up emceeing the media conference and launch of the 2018 Australian Transplant Games, at the Super Sports Centre, Runaway Bay. This launch also marked the start of our 3-day High Performance Training Camp. The Queensland Government is a major supporter of the Transplant Games, to be held here on the Gold Coast September 30-October 6. Health Minister, The Hon. Dr Steven Miles spoke of how this event would increase awareness and hopefully an upward swing in organ and tissue donation.
Following the official proceedings, we split into our respective sports and hit the track or pool. That first session under the guidance of Coach Stephen Howell was the most alive I have felt in years. Although I’ve been back in the water for a while, the challenge and absolute thrill of having a go really got my heart pumping! I sucked in some big breaths with each lap and as I smashed the wall at either end of the pool, I looked around and thought about my fellow transplant athletes. While my body and its organs, is now running on someone else’s stem cells, some of them had someone else’s heart or lungs helping them reach the end of the pool. Whoa……. I said some silent, but powerful thanks to our donors, their families and our medical teams. The emotions were running high, but while there was a little rest between sets, there wasn’t too much time to lose focus. While Steve pushed us hard, he also had us laughing. Like when he nicknamed young Logan ‘donkey’, as a term of endearment. Steve explained that when he saw real potential in a swimmer he’d ride them like the last donkey in town. Nuff said.
We enjoyed team meals in the dining hall, surrounded by international athletes in town preparing for the upcoming Commonwealth Games (including the Indian basketballers like ‘One in a Billion’ Satnam Singh! who graciously posed for a pic and hilariously high-fived/low-fived me when we passed between our rooms and training sessions:-). The vibe was sensational. The conversation covered everything from heartbreaking transplant wait-list experiences, to inspirational tales of recovery and determination to really live (like they say, ‘no-one lives like the dying’). I wished I could bottle this. Not just for my darker moments, but for anyone who might find themselves needing a little light at the end of the proverbial tunnel.
My ‘body scans’ went from analysing the pain, its severity and what medication I could take to try and control it, to how my muscles were feeling having worked harder than they had in a long, long time. I doubted whether I could keep up, but despite the hurt and exhaustion, was set on living up to the hashtag I started using during my transplant #stillkickin. In this case, I literally was still kicking!!
We were imbued with knowledge from experts during Strength and Conditioning (Adsy Gordon), Nutrition (Travis Ronaldson) and Sports Psychology (Craig Pearman) sessions. A lot of us struggle with fatigue just getting through the day, so this lecture format side of things was at times, quite tiring. The information though – so beneficial.
A key point of discussion was Internal and External motivation. A room full of people who have survived, and are thriving after transplant, perhaps don’t need to be taught about internal motivation. Without it, we all may have rolled over, given up, quit. It’s that beautiful combination of internal and external motivation that has created success. I heard so many stories of athletes not wanting to let their family, donor family or Dr’s down. It’s a powerful mix.
Speaking of power…we were gifted a very special insight into world class competitive swimming, with visionary of the sport, Bill Sweetenham. As a mad-keen young swimmer I watched some of his pupils including Tracey Wickham, power to glory on the Olympic stage. Bill’s name is synonymous with some of the most successful international teams in history. I was shaking like a leaf when I entered the ‘Elite Room’ and reached out to shake the hand of greatness. There he sat, in an empty room, just his big hat and dark sunnies and a bucketload of stories to share. I could listen for the rest of my days, but we soon found our way to the pool deck. Holy hell. I was so bloody nervous to strip down to my togs and hop in, I had to go and tell him I was terrified! All of a sudden my head had forgotten how to swim. As Bill took a seat laneside, we all slowly settled into our groove. Before too long, he had us all lined up, hanging onto the side of the pool listening intently to little tweaks we could each make. Teenage transplant recipient Claudia was given the somewhat unenviable task of jumping out to demonstrate getting full reach from a stroke. Whilst manipulating body position in that way, in front of all of us may have been daunting – Claude handled it like a pro, and I winked at her Mum Anna saying “she’ll never forget this.” None of us will.
Bill generously shared more stories with us (as we recovered from a session in the ice baths – another first for some of us!), he detailed the importance of balance and fun. What a way to cap off an unbelievable afternoon!
Some participants opted to sleep in on the final morning (totally cool given the workload and long days), while others managed a final hit out. I’m happy to say that although my body was screaming with pain – it was great pain – and I was in the water by 6 am. The mental chatter was strong, but there was no way I was missing this last opportunity. Apart from Coach Stephen giving us drills we could test, then take away, he’d also built enough confidence in our group to critique each other. The kindness and positive feedback was palpable. How all of us will grow as a result. I am so excited for the Games!
I grew up swimming, enjoyed training and loved to compete. I can’t say I ever had fun in the water though. That said, it is my ‘happy place’. I can float on my back for hours. Having been hooked up to machines to keep me alive, I revel in the freedom. The cold rush as I dive in, the swoosh of the water passing my ears, the exhilaration I feel powering along the black line and the absolutely life-affirming satisfaction at hitting the wall. Fun though? Nope, not really. Until the other day. The last few minutes of our swim session, Coach Steve suggested a Michael Phelps drill for vertical kick training (you’ve gotta watch this!). Ahhhh, yeah, right. Well, getting out into the middle of a lane, dropping till your feet are flat on the bottom, then squatting, pushing up, streamlining and butterfly kicking up out of the water like a rocket is unreal! Such an incredible feeling. And yes, I had FUN!
The reality of organ and tissue donation is very simple – people that were once terminally ill, are now here.
CEO of Transplant Australia, Chris Thomas provided this example at the launch of the Games and start of the High Performance Camp, going around the group asking ‘years since transplant?’ In a staggering display, we added up the numbers and we, those of us gathered who had been granted this precious gift, have so far enjoyed an additional 266 years of life. That is a whole lotta birthdays, anniversaries, children and other milestones that may not have been.
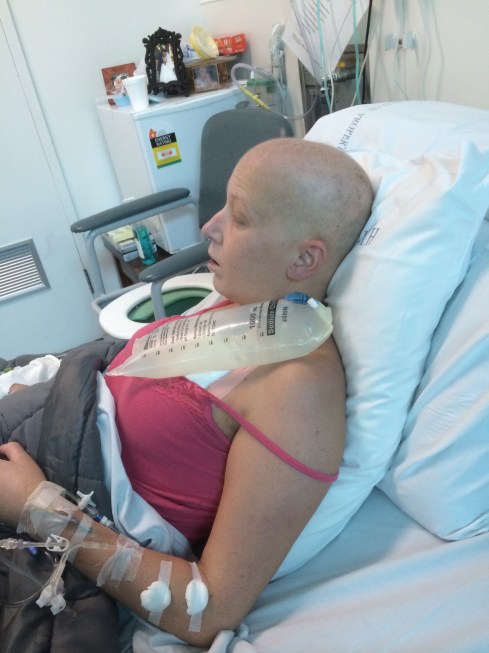
Although the post-transplant life is very much filled with medical appointments, medication and a multitude of side-effects, it is life. Life that, if not for our donors, we could not sustain. I feel strongly it is my duty to honour my anonymous donor and my team, by looking after this body post-transplant, and live the best life I possibly can. Thank you, may never be enough.
I encourage anyone reading this, who hasn’t had the conversation about organ and tissue donation with their loved ones, to please do so. Your decision can and will save lives.
Make the decision count – donatelife.gov.au
Huge thanks to Nick Farley for some of the above images. Check out the rest of the HPC via his Insta farleyphotographix